Tweetchats have become very much more difficult to run, as we cannot get transcripts, analytics are troublesome and Tweetdeck is a paid for function of Twitter (X). So in December 2023 we asked you if you wanted the Physiotalk tweetchats to continue – and the polling suggested this was the case, but to move to […]
physiotalk
Making the most of social media to learn, share and influence.
Your HCPC renewal #physiotalk Monday 15th Jan 8pm
Our first chat of 2024, and the first under our new monthly calendar will be on the topical question of HCPC renewal. Yes – it is that time of year (or two years..) again! The tweetchat will use our usual hashtag of #physiotalk and we be for an hour from 8pm on Monday 15th January […]
Behaviour change #physiotalk 22nd May 8pm
The #physiotalk tweet chat on Monday 22nd May at 8pm BST is all about behaviour change. There is overwhelming evidence that changing people’s health-related behaviour can have a major impact on some of the largest causes of mortality and morbidity, so it is vital that physiotherapists have behaviour change knowledge that they can use to […]
Practice Based Learning in Private Practice #physiotalk 19th June
Our chat on 19th June is being hosted by Laura Smith, @lo_physio. Laura is a Workforce Transformation Fellow at NHS England; her work is looking at AHP Nursing and Midwifery placement expansion in non-NHS Settings. Laura will be working with two students @physio_muskan and @PhysioMar on placement in June who will help develop this chat […]
The NHS strike #Physiotalk Monday 30th January 8pm
Today (Thursday 26th January) physiotherapists across England took the unprecedented action of going on strike for fair pay. Physiotalk stand in solidarity with the striking staff and we are going to focus Mondays tweetchat on the strike, what it hopes to achieve and how those striking felt about taking part. So join us on Monday […]
Establishing a Dementia Network #physiotalk Mon 5th December
Our next chat will be on Monday 5th December at 8pm GMT. It will be hosted by @AGILECSP. AGILE writes ‘On Tuesday 29th December 2022, AGILE and the Chartered Physiotherapists in Mental Health (CPMH) held our first meeting of a new ‘Dementia Network’ for physiotherapists working in this field or with an interest in dementia […]
The NHS pay dispute and ballot #physiotalk 7th Nov 8pm
I’m typing this towards the end of October when the country is in a state of turmoil again following the resignation of Liz Truss as Prime Minister. Events are moving so fast I am almost hesitant to type up a post for our next #physiotalk tweetchat on Monday 7th November at 8pm GMT. On Monday […]
Supporting new graduates #physiotalk Mon 29th August 8pm
Our next chat is on Monday 29th August at 8pm BST. Yes – we know it is a bank holiday for many people, but we would love it if you could spare an hour to chat about this important topic. Over that last couple of months hundreds of new physiotherapists will have started their first […]
#AHPsActive travel – a #physiotalk tweetchat Monday 1st Aug 8pm
The date of our next #physiotalk tweetchat is Monday 1st August at 8pm BST. But the 1st August is also the start of the now annual #WeActiveChallenge when a variety of health care professionals compete against each other to be the most active in August – the type of competition where we all win! We […]
What is ‘good rehabilitation’ #physiotalk Monday 4th July
Tempting as it was to join our cousins across the pond in a 4th July celebration, we have decided to stick with our usual Monday night tweetchat at 8pm BST! The topic is linked to the publication of Rehabilitation and Recovery: A Once for Scotland Person-Centred Approach to Rehabilitation in aPost-COVID Era We are not […]
Are you able to provide the slow stream rehabilitation that many older people with deconditioning require? #physiotalk 6th June
Our next chat is with AGILE – Chartered Physiotherapists working with Older people, @AGILECSP. It will be on Monday 6th June at 8pm BST – as usual just follow along using the #physiotalk hashtag. As a result of the COVID-19 pandemic, a new healthcare problem has become increasingly evident amongst our older adult population – […]
#Physiotalk 200: The Big Debate 9th May 8pm BST
This is the big one: after starting in December 2013 we have reached our 200th tweetchat! When Naomi and Janet dipped their toes into tweetchatting it was all a bit of an experiment. Now here we are 199 chats in and over 300 million tweet impressions later, plus a research project or two! We are […]
Physiotherapy and strength training #physiotalk 25th April 8pm BST
Our next #physiotalk tweetchat will be on Monday 25th April at 8pm BST. The topic will focus on strength training in physiotherapy – a hot topic at the moment with the recent launch of the CSP ‘Stronger my way’ campaign. However, we will not be discussing the campaign specifically – more the general principles of […]
Clinical-academic research and career pathways #physiotalk 11th April 2022 8pm BST
Our next tweetchat is on Monday 11th April 2022 at the usual time of 8pm BST Hosted by Samuel Stuart (on behalf of Physiotherapy Research Society) @PhysioResSoc / @samstuart87 Physiotherapy Research Society (PRS) The Physiotherapy Research Society (PRS) is a Professional Network of the Chartered Society of Physiotherapy and is for all physiotherapists, particularly those […]
Weight management and physiotherapy #physiotalk 28th March 8pm BST
Our next tweetchat is on Monday 28th March at the usual time of 8pm BST – note that the clocks will have changed if you are joining us from outside of the UK! It is being hosted by @physioNT and is all about weight management. Guidance from the National Institute for Health and Care Excellence […]
HCPC re-registration #Physiotalk 8pm GMT 14th March 2022
Physiotherapists in the UK are required to re-register with the Health and Care Professions Council (HCPC) every 2 years. The renewal window for Physiotherapists opened on 1st February 2022 and closes on 30th April 2022. The focus of the #Physiotalk on 14th March is registration with the HCPC. Tonight we will be discussing the standards […]
Support workers: Unregistered NOT unqualified #physiotalk Mon 28th Feb
The next #physiotalk tweetchat is on Monday 28th February 2022 at 8pm GMT. It is being led by a group of passionate physiotherapy support workers @chris_richards2 @gvhawtin @LorraineAllchu2 and @SherylB76 They aim to discuss the role of the support worker and their values. They would like to know in what ways are support workers supported? […]
Physiotherapy Declares a climate emergency and… #physiotalk 17th January
Following on from the #physiotalk chat with @PhysioSusNet talk, COP26 and 2021 reports, health is now on the climate change agenda. We are pleased to welcome @physio_declares to host this tweetchat on Monday 17th January at 8pm GMT “Code red for humanity” – UN secretary General Just as we have seen with international responses to […]
Physiotherapy for people living with dementia – what works? #physiotalk 6th Dec
Our next tweetchat is on Monday 6th December at 8pm GMT. It is guest hosted by @AGILECSP and will look at the topic of physiotherapy for people living with dementia. Dementia is an umbrella term for a range of conditions including Alzheimer’s disease, vascular dementia, Lewy body dementia, frontotemporal dementia and mixed dementia. There are […]
Common Placement Assessment form #Physiotalk 8th Nov 2021
The next #physiotalk tweetchat will be on Monday 8th November at 8pm GMT The topic is the new Common Placement Assessment form which has been developed by the CSP. They say that ‘the Common Placement Assessment Form (CPAF) is a standardised assessment form that can be used to assess all physiotherapy students out on placement […]
Support workers and scope of practice #physiotalk on Monday 11th October
The next #physiotalk tweetchat is on Monday 11th October at 8pm BST. This weeks topic is ‘Support workers and scope of practice’. Support workers, senior support workers, assistants, assistant practitioners – what ever they are called, most of us work alongside support workers and they are invaluable members of our teams – we really couldn’t […]
Your professional body and you #physiotalk Mon 16th Aug 8pm
7.3% 7.3% was the turn out in the recent Chartered Society of Physiotherapy Council elections. That’s just over four thousand members voting out of a membership of nearly sixty thousand physiotherapists, students and associate members. Does that surprise you? Are you concerned about the lack of engagement with the election? Or are you not particularly […]
#AHPsActive tweetchat #physiotalk Mon 2nd Aug 8pm
It’s August – and so of course that means the return of the #WeActiveChallenge We hope that you started posting your #AHPsActive photos on 1st August – and if you are reading this wondering what I am talking about, then take a look at the We Communities website to find out more (and of course […]
The gender (im)balance in physiotherapy #physiotalk Mon 5th July 8pm
The next tweetchat will be on Monday 5th July at 8pm BST. The topic is on the gender balance (or possibly imbalance) in physiotherapy and how this is changing over the years – has this changed the profession and how it might be perceived outside of physiotherapy. World Physiotherapy report on each of their member […]
Physiotherapy, Research and Older People #physiotalk Mon 19th July
The tweetchat on Monday 19th July at 8pm BST is hosted by @AGILECSP AGILE is a Professional Network of the Chartered Society of Physiotherapy and is for therapists working with older people – whether qualified physiotherapists, assistants, students or associate members of an allied profession. AGILE’s mission is ‘To deliver the highest possible physiotherapy practice […]
CSP council election tweetchat Mon 21st June 8pm BST
With apologies for those Physiotalk followers outside of the UK, our tweetchat on Monday 21st June at 8pm BST will be focused on elections for the Chartered Society of Physiotherapy (CSP) council. The ballot papers are out and the candidates statements are all available for you to read either from the booklet you are sent […]
Sustainability in Physiotherapy #physiotalk 10th May
The next #physiotalk tweetchat is on Monday 10th May at 8pm BST and is guest hosted by @PhysioSusNet: The Physio Sustainability Network is for those interested in sustainability & reducing the physiotherapy carbon footprint. The scale of the problem The World Health Organization has described climate change as “the greatest threat to global health in the 21st century” and […]
The impact of COVID-19 on rehabilitation services for older adults #physiotalk 29th Mar
The next #physiotalk tweetchat is on Monday 29th March at 8pm BST Four of the Chartered Society of Physiotherapy Professional Network’s have teamed up to discuss the impact COVID-19 has had on rehabilitation services for older adults @AGILECSP, @theACPRC, @PhysioATOCP and @ACPICR. This has allowed us to cover the full spectrum of rehabilitation specialities in […]
COVID 19 – Self care and avoiding burn out #physiotalk Mon 15th Mar 8pm
The next #physiotalk tweetchat will be on Monday 15th March at 8pm GMT- Grab a cuppa of whatever takes your fancy and join us in a bit of self care. More and more physiotherapists are reporting signs of burnout, and is it any surprise? We know large numbers of health care workers are feeleing the […]
COVID 19 – Transferable skills #physiotalk Mon 1st Mar 8pm
The next #physiotalk tweetchat will be on Monday 1st March at 8pm GMT – or as its known in our household – St Davids day! So first – have your cawl and welsh cakes (and if you don’t know what I’m talking about – take a look here!), then join us for a tweetchat all […]
CPD essentials #physiotalk Mon 1st Feb 8pm GMT
The people have spoken – or at least a twitter poll did! The top choice for our next chat is to look at CPD essentials. So that is what we will focus on during the tweetchat on Mon 1st Feb at 8pm GMT. Those of you with long memories may remember that one of the […]
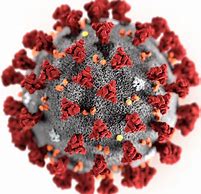
#LongCOVID – what is the role of the physio? #physiotalk 19th October
This #physiotalk tweetchat will take place on Monday 19th October at 8pm BST. At the start of the pandemic we had chats on our urgent responses to the COVID crisis – PPE, respiratory care, rehabilitation after ICU. Now we are settled into our roles in these areas, we know what to do even as a […]
Support After COVID #physiotalk Mon 5th October
We are hosting a physiotalk that is part of a research project – the Support after COVID study @SupportAfterCo1. The chat will be on Monday 5th October at 8pm BST. There will also be an identical chat by the We Communities team using #WeMDT on Monday 28th September as the research team are aiming to […]
Dementia and physical activity #physiotalk 21st Sep
Lets talk about Dementia! Our next #physiotalk tweet chat on Monday 21st September at 8pm BST will focus on physiotherapy, dementia risk and exercise for those living with dementia. Its not the first time we have chatted about dementia, but since the last one was six years ago, it seemed like a good time to […]
Getting active #physiotalk Mon 10th Aug 8pm
Its August – and so of course that means the return of the #WeActiveChallenge We hope that you have been posting your #AHPsActive photos since the start of August – and if you are reading this wondering what I am talking about, then take a look at the We Communities website to find out more […]
Physiotherapy and Cooking #physiotalk 13th July 8pm
Are physiotherapists in a prime position to promote the vast benefits of cooking? That is the question our guest host Ben Rowles is asking ahead of our #physiotalk tweetchat on Monday 13th July at 8pm BST Physio.Kitchen is about encouraging people to cook. From a physiotherapy perspective, cooking has a wide range of benefits similar […]

Covid-19 and virtual placements: what does good look like? #physiotalk Monday 29 June
As part of our ongoing Covid-19 series, our next tweetchat on Monday 29th June will focus on ‘virtual’ placements in physiotherapy and other health, public health and social care services in the pandemic response and for future care. Digital health Digital healthcare had been a policy priority in many countries for some time now, but […]
Primary Care and Community MSK Services: Post-COVID #physiotalk 15th June
The Physiotalk tweetchat on Monday 15th June is on ‘Primary Care and Community MSK services: how are you coping and how will your service have changed post-COVID19?’ and is guest hosted by @ChrisMartey As usual it will be from 8pm BST and we look forwards to people joining using the hashtag #physiotalk for the chat. The […]
Diversity within Physiotherapy #physiotalk Mon 8th June 8pm BST
The tweet chat on Monday 8th June at 8pm BST has been suggested by Emmanuel Ovola @Manni_O who asks ‘How does lack of diversity affect the minority populations in Physiotherapy?’ The lack of diversity in physiotherapy is having a direct impact on BAME communities. The issues encountered starts within physiotherapy pre-registration education, with a study […]
COVID19 #Physiotalk – The impact on private practice Mon 25th May
Our series of Monday nights tweetchats focussed on issues linked to COVID19 continues this Monday 25th May at 8pm BST The focus this week is on the impact on private practice – an area of physiotherapy practice that has been especially hard hit during the pandemic. However, many clinics and practitioners have been fantastic innovators, […]
Recovery planning: creating lasting change from Covid-19 #Physiotalk Mon 18th May 8pm BST
As the pandemic progresses international, national, and regional attention is turning to focus on living with Covid-19, the ‘new normal’; and restarting of business and usual work. The acceleration of change and innovation within health and care as a result of the pandemic response has created important conversations about what needs to to stop/start/continue in […]
COVID19 #physiotalk – A respiratory update Mon 11th May 8pm
We moved to weekly chats in the light of the COVID19 pandemic on 23rd March – and it feels that a lot has progressed since then. Our chat on 23rd March had a focus on respiratory issues – but at that time there were only a handful of physiotherapists on the chat reporting they had […]
COVID19 and your own wellbeing #physiotalk 4th May 8pm
It has often been said that the time we are living through at the moment is unprecedented. Whatever your role in physiotherapy you are likely to have faced huge changes in where or how you work. This has the potential to take a toll on your mental health and wellbeing. The #physiotalk tweetchat on Monday […]
Rehab and COVID19 #physiotalk Mon 13th Apr 8pm
Our next chat is on Monday 13th April at 8pm BST. We normally have an Easter Monday special, but instead we are continuing our COVID19 themed chats. We know this Easter will be very different in many ways, and it seemed more important to continue supporting you in sharing knowledge about COVID19 than searching for […]
COVID19 #physiotalk on PPE Mon 6th Apr 8pm
In last weeks #physiotalk questions were raised about Personal Protective Equipment or PPE. Our next #physiotalk chat at 8pm BST on Monday 6th April will be focussing on the right PPE to support physiotherapists working on the frontline of the battle against COVID19 – whatever your setting. Updated guidelines have been produced on 2nd April […]
COVID19 #physiotalk with @theCSP Mon 30th Mar 8pm
In a crisis such as the current one, many physiotherapy staff turn to their professional body and trade union for help. @TheCSP staff have been working round the clock to ensure their members get the advice and guidance they need to navigate the extraordinary circumstances in which they find themselves. This ranges from how to […]
COVID19 chat #physiotalk 23rd March 8pm
We are moving from our usual fortnightly chats to offer an extra chat on the topic that we are all talking about – COVID19 and Coronavirus. We asked you if you wanted a chat – and you said yes. We asked you what you wanted to start with – and you said looking at how […]
Getting your abstract written for Physio UK #physiotalk 16th March
The tweetchat on Monday 16th March will be focussed on how to successfully submit an abstract – and in time for #Physio20! Join us at 8pm on Monday 16th March by using the hashtag #physiotalk to search for tweets and use in your tweets. Not tweetchatted before – don’t worry there is lots of information […]
2020 Vision for #physiotalk Mon 6th Jan 8.30pm
Physiotalk has just had its 6th birthday and over 130 chats later we are entering a new decade and we thought it was time to have a think about the role and purpose of Physiotalk. Social media has grown and developed since the 16th December 2013 and perhaps its time for Physiotalk to take a […]
The Great Big #physiotalk Christmas and Birthday quiz! 16th Dec 8.30pm
Our next #physiotalk tweetchat isn’t a chat at all! We thought as the 16th December marks exactly 6 years since our first ever Physiotalk, on 16th December 2013, then we should get into a festive and birthday mood! So instead of a chat, on 16th December we are going to hold the ‘Great Big #physiotalk […]